Bianca Barea
Consultant Urologist, Beaumont Hospital
Consultant urologist Dr Bianca Barea discusses the importance of shared decision-making for bladder dysfunction and the life-changing intervention of sacral neuromodulation.
Urinary and faecal incontinence affect millions, yet stigma and embarrassment mean many never seek help or discuss their symptoms,” says Bianca Barea, consultant urologist at Beaumont Hospital. “Patients need to know that treatment options are available, empowering them to take that first step to initial assessment.”
Raising awareness of sacral neuromodulation
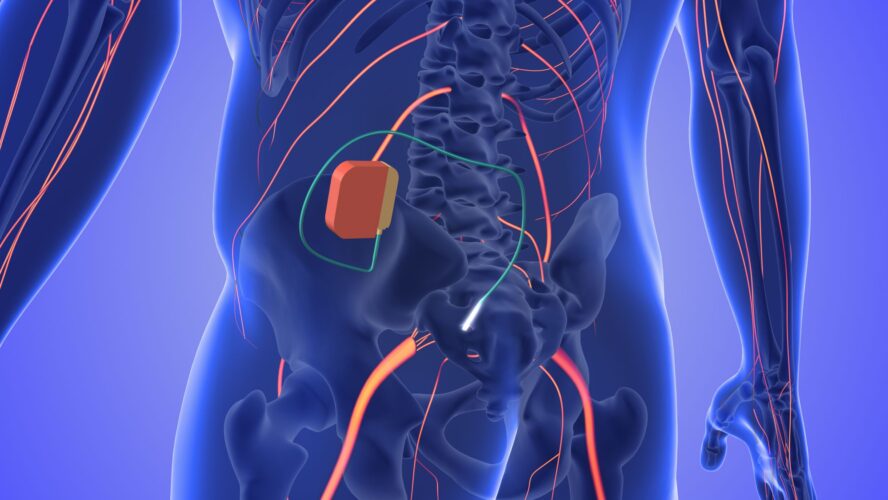
Sacral neuromodulation (SNM) is a minimally invasive procedure in which an implanted device sends mild electric impulses to stimulate the nerves that control your bowel and bladder. “Alternative treatments for bladder control often require repeat procedures, but the SNM device can last for many years, providing long-term relief, giving patients their quality of life back,” explains Barea.
“SNM is typically a third-line option for patients who haven’t responded to conservative or medication-based treatments, but it can be life-changing, helping patients regain normal bladder or bowel function. Patients who undergo the SNM procedure often report dramatic improvements; some go from waking five times a night to not waking at all, or from being unable to void to emptying normally again.”
Beaumont Hospital has a comprehensive SNM service, including a highly experienced team — Dr Barea, Dr Forde, Dr McCawley and advanced nurse practitioner Hannah Graham — equipped to provide patients with expert assessment, individualised treatment planning and seamless management of both trial and permanent SNM implants. “We also run workshops for GPs to ensure they know that SNM is an option for patients in practice.”
Sacral neuromodulation (SNM) is a minimally invasive procedure in which an
implanted device sends mild electric impulses to stimulate the nerves that control your bowel and bladder.
Importance of shared decision-making
Shared decision-making is important, aligning treatment discussions with the expertise of the healthcare professional and the patient’s preferences. “Making patients aware of their treatment options is one of the most important parts of the consultation,” explains Barea. “Each treatment option has its pros and cons, and what’s right depends on the patient’s age, gender, lifestyle and the specific characteristics of their condition. Patient preferences are key, and treatment should be tailored to everyone’s needs.”
Raising awareness of potential treatment options can influence patient outcomes, whether through information aids such as leaflets or via online resources such as BAUS or BBUK, which ensure that patients fully understand their choices, feel supported in decision-making and can access the most appropriate therapies for their individual needs.