
Professor Sinead McGilloway
Centre for Mental Health and Community Research, Maynooth University Department of Psychology and Social Sciences Institute

Mary Cronin PhD
Centre for Mental Health and Community Research, Maynooth University Department of Psychology and Social Sciences Institute
The well-being needs of carers health continue to go unrecognised. One in five people in Ireland will be providing care to a loved one by 2030.
Ireland’s population is ageing, which means that a growing number of people are living with dementia and other chronic conditions. People with disabilities are also living longer.
Thus, many of our most vulnerable citizens depend heavily on the unpaid work of family carers. Through their selfless and often unrecognised work, they save the state billions of euro annually. According to the CSO Irish Health Survey, 10% of the population over 16 are carers.
The caring experience
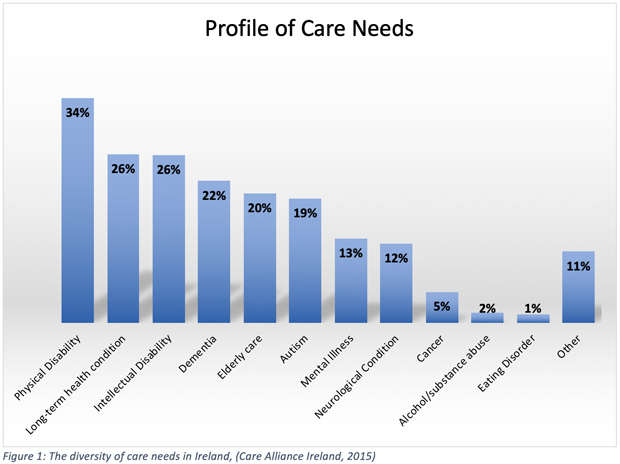
Providing care to a loved one can be rewarding for family members, but it is not without its challenges. However, family-member carers are often not equipped to meet all of their needs (see Figure 1). Furthermore, the demands of the caring role mean that carers often have little time to look after their own health.
Carers experience poorer physical and mental health than the general population; the demands of the caring role can leave them physically exhausted and emotionally isolated.
Carers’ wellbeing is often misunderstood
The public regard carers highly (as exemplified by the recent ‘Carer of the Year’ awards). However, many report that their communities do not typically understand, the challenges of caring and its impact on the carer. Carers are asked frequently about their loved one, but are rarely asked about their own health and wellbeing.
Feeling invisible as a carer
On a related point, despite the carer advocacy work of organisations such as Family Carers Ireland and Care Alliance Ireland, many carers report feeling undervalued, overworked and under-supported. Indeed ‘invisible’ is often a word they use to describe themselves and the challenging work they do. This invisibility of carers is likely to continue if we do not initiate a conversation about caring with all relevant stakeholders. These include health and social care professionals.
Changing our policy on carers
Recent years have seen an increasing focus on community healthcare. These have been through the development of primary care centres in many areas around the country. Thus, health services may now be better placed to support vulnerable groups in the community such as carers. However, healthcare professionals must understand carers needs, and help them with support and consultation.
Thinking of the patient and the carer
One possible solution to this challenge would be to provide awareness-raising events and training for health care professionals regarding the needs of carers. For example, in Australia, a programme called ‘Think Patient, Think Carer’ encourages primary care services to consider the needs of carers who may be supporting a person with a chronic condition.
Likewise, in England, the Royal College of General Practitioners has developed a toolkit and ‘Action Guide’ to help GPs better support carers. To date, no such community health initiatives exist in Ireland to support the health and wellbeing of carers at a national level, thereby indicating a yawning gap in current provision.
The team at the Centre for Mental Health and Community Research, Maynooth University Department of Psychology, aims to address this gap in an Irish context by identifying the facilitators and barriers to the implementation of a community healthcare approach, whilst also investigating perceived carer stigma and training of health care professionals.
The development of, for example, practice guidelines and training will be informed by these findings. Carers will get support in appropriate, timely and effective ways by implementing this at a national level. The early findings of this research will be available in late 2019.

